Incidence, susceptibility and outcomes of candidemia in adults living ... - BMC Infectious Diseases
Incidence
Overall annual incidence of candidemia among patients living in the CZ was 3.8 per 100,000 population, ranging from 3.2 per 100,000 in 2012 to 5.0 per 100,000 in 2014 (P < 0.001; Fig. 1). Incidence changed throughout the study but did not differ between start and end (P = 0.54). The annual incidence among patients between 0 and 39 years was generally low, ranging between 0.2 and 1.8 per 100,000, and increased during the study period (P < 0.01) (Fig. 1). The annual incidence among patients between 40 and 59 years was steadily low and ranged between 3.3 and 7.1 per 100,000. The annual incidence among patients between 60 and 79 years and > 80 years fluctuated more and was higher, ranging between 8.7 and 17.8 per 100,000 and 8.0–29.9 per 100,000, with no significant changes over the study period.
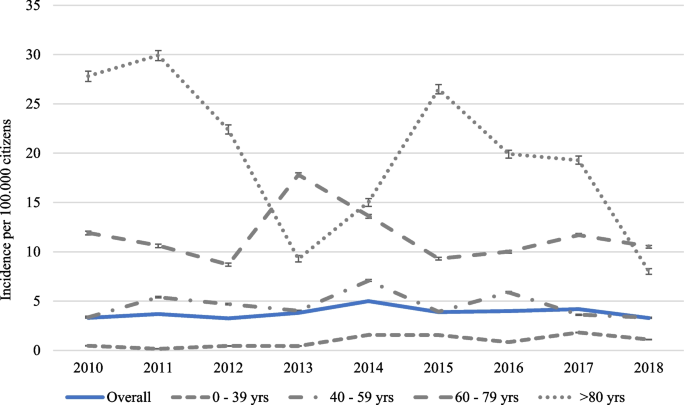
Overall annual incidence of candidemia per 100,000 citizens among individuals in the Calgary Health Region, and the annual incidence per 100,000 citizens among individuals 0–39 years, 40–59 years, 60–79 years and > 80 years between 2010 and 2018
Patient demographics
In total, 455 individuals with 466 episodes of candidemia were analysed. Patients with multiple episodes had events separated by 692 days (IQR 403–852). Median age was 61 years (IQR 48–72), ranging from 19 to 100 years, and 47.4% of the patients were female (Table 1). Median hospital stay was 28 d (IQR: 14–55 d), ranging from 0 to 1470 d, with 53.7% getting ICU support. In total, 16.7% of patients were transferred to CZ from another hospital; based on postal code, 44 non-Calgary residents were excluded from incidence calculations. Most patients were discharged from the hospital (54.9%), 42.1% died before discharge and some left the hospital against medical advice (2.6%) or were transferred to another hospital (0.2%). Most (n = 366, 78.5%) patients were treated with antimicrobials 30 d before candidemia, approximately half (48.5%) had cardiovascular disease as a comorbidity and approximately one-quarter had diabetes, chronic liver disease, pulmonary disease, or cancer (Table 1).
Candidemia
Approximately 23.4% of Candida bloodstream infections were community acquired, with the remainder hospital acquired. Overall, patient demographics were similar between groups, although patients with hospital-acquired candidemia were more likely to have cardiovascular disease (51.3 vs. 39.5%; P = 0.03), specifically congestive heart failure (17.7 vs. 4.6%; P < 0.001) and arrhythmia (27.5 vs. 11.0%; P < 0.01), but less likely to have peripheral vascular disease (3.6 vs. 10.0%; P = 0.01). In addition, hospital-onset candidemia more often had cancer in the last year (25.8 vs. 14.7%; P = 0.02), were receiving parenteral nutrition (20.7 vs. 1.8%; P < 0.001) or received ≥ 10 mg prednisone equivalent of corticosteroids daily for the last 30 days (30.3 vs. 15.6%; P < 0.01)[20]. Asthma was more apparent in community-onset candidemia infections (9.2 vs. 3.9%; P = 0.03) (Table 1).
The most common isolated species were C. albicans (50.6%) and C. glabrata (24.0%) (Fig. 2). An infection with a second and different species of Candida isolated > 2 d after the first positive culture occurred in 5.8% of the cases. In 32% of these cases, patients got an infection with C. albicans and C. glabrata. No other trends were observed. The relative proportion of the six most common Candida species (C. albicans, C. glabrata, C. parapsilosis, C. dubliniensis, C. krusei and C. tropicalis) did not change over time, apart from a transient decrease in C. albicans between 2010 and 2012 (P = 0.02) and a significant increase in C. glabrata infections (P = 0.03). (Fig. 3).
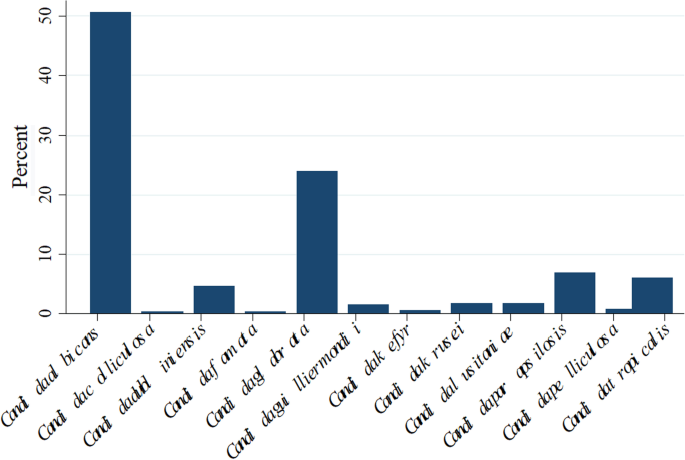
Distribution of species causing candidemia between 2010 and 2018
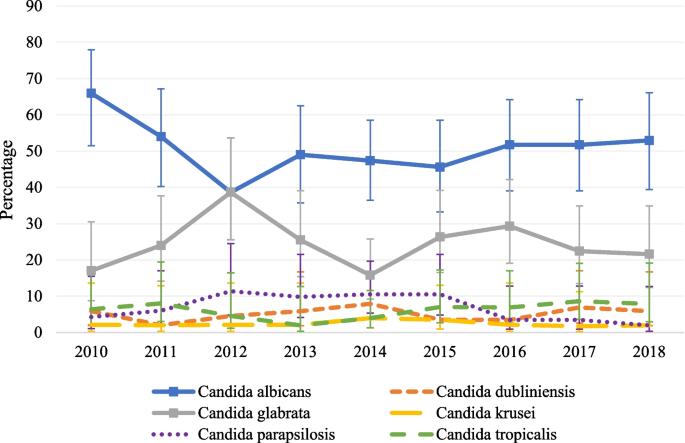
Relative proportion with 95% confidence intervals of Candida species causing Candida bloodstream infection each year, over time between 2010 and 2018
Mortality
Forty-four (9.4%) of patients with candidemia died within 24 h after the index blood culture and were excluded from analyses. For the remaining 422 patients, all-cause mortality rate at 30 d, 90 d and 1 y post candidemia was 32.2% (95% CI: 27.7–36.7%), 40.1% (95% CI: 35.4–44.8%) and 48.1% (95% CI: 43.3–52.9%), respectively. The all-cause mortality rate at 30 d, 90 d and 1 y post candidemia was generally higher in the patient group with hospital acquired candidemia infections than the community-onset group (35.7 vs. 21.0%, P < 0.01; 42.6 vs. 32.0%, P = 0.06, and 51.9 vs. 36.0%, P < 0.01). When stratifying mortality by the three most common Candida species, the all-cause mortality rate at 30 d, 90 d and 1 year post candidemia did not differ from the overall rate. For C. albicans (n = 218 patients), mortality at 30 d, 90 d and 1 year were 32.1% (95% CI: 25.9–38.3%), 38.5% (95% CI: 32.0–45.0%) and 45.4% (95% CI: 38.8–52.0%), respectively. For C. glabrata (n = 106 patients) mortality at 30 d, 90 d and 1 year were 34.0% (95% CI: 25.0–43.0%), 43.4% (95% CI: 34.0–52.8%) and 55.7% (95% CI: 46.2–65.2%). Finally, for C. parapsilosis, mortality at 30 d, 90 d and 1 year were 26.5% (95% CI: 11.7–41.3%), 38.2% (95% CI: 21.9–54.5%) and 44.1% (95% CI: 27.4–60.8%).
Documented blood culture clearance of Candida spp. from blood occurred in 343 patients, with a median duration of candidemia of 4 d (IQR 2–6 d). Furthermore, 84% of patients cleared their Candidemia in < 7 days (Fig. 4).
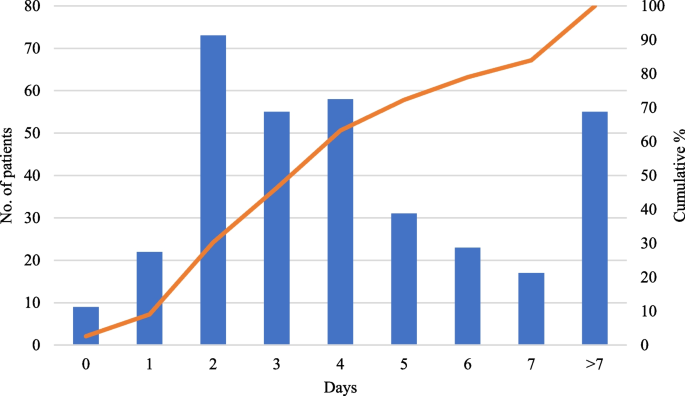
Length in days between first positive and first negative culture for 343 patients with documented clearance of Candida spp. from blood
Average interval from hospital admission to candidemia diagnosis was 16 d (95% CI: 13–20 d) with a median of 8 d. Readmission within 1 y occurred in 102 patients (21.9%), but this was due to candidemia in only 5 patients (4.9%).
Nine (2.0%) patients had two or more distinct episodes of candidemia during the study period but were classified as unrelated. Most were admitted twice, and 2 were re-admitted 3 times. For these 9 patients, median interval from discharge to readmission was 599 d (IQR 403–852 d), ranging from 48 to 2,026 d.
Antifungal susceptibilities of Candida species causing candidemia
Susceptibility testing was performed for all isolates of C. albicans (n = 242), C. glabrata (n = 117), C. parapsilosis (n = 33) and C. tropicalis (n = 30). Resistance to common antifungals ranged from 0 to 2.5%, and percentage of non-wild types from 0.0 to 9.4% for C. albicans (Table 2). These percentages were slightly higher for C. glabrata (1.0–9.4% and 0.0–7.8%) (P < 0.01; P = 0.63; Table 3) and higher for C. tropicalis isolates ((0.0–31.0% and 0.0–52.9%) (P < 0.001; P < 0.001; Table 4)). No resistance was observed for C. parapsilosis (Table 5). No difference in percentages of susceptible dose dependent (SDD and resistant isolates was observed among the 4 hospitals, except C. glabrata isolates resistant for fluconazole decreased from 5.1 (95% CI: 1.9–10.8%) to 1.2% (95 CI: 0.0–46.9%) after removing one site from the equation (this site had much higher local resistance than the other three sites).
Comments
Post a Comment