The bacteria that may trigger multiple sclerosis - News - The Rockefeller University
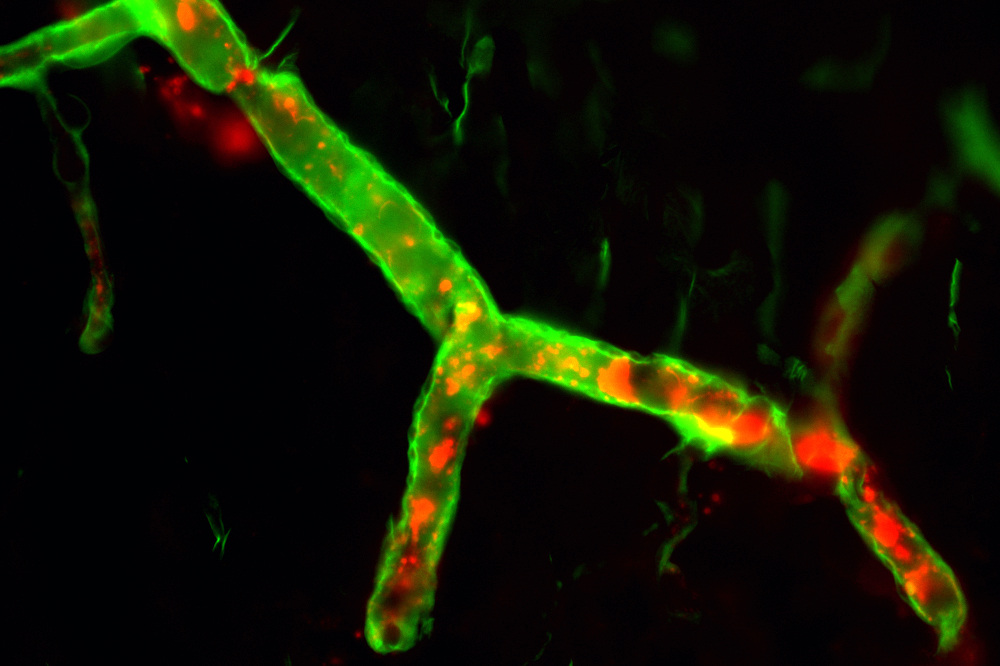
A C. perfringens toxin (red) can bind to the blood vessels of the central nervous system (green), potentially triggering MS.
A common microbe found in sewage, marine sediment, soil, and the GI tracts of pets and farm animals may play a defining role in multiple sclerosis, according to a new study. The findings, published in The Journal of Clinical Investigation, suggest that a toxin produced by certain C. perfringens bacteria may be the long sought-after trigger that degrades the blood-brain barrier and kicks off the relentless inflammation and brain cell degradation characteristic of MS.
"If this is the environmental trigger for MS, we can now start talking about a vaccine, monoclonal antibodies, or some other therapy," says Rashid Rumah, co-author of the study and a physician scientist in Vincent Fischetti's lab at Rockefeller.
An estimated 2.5 million people are living with multiple sclerosis, and about 200 new cases are diagnosed each week in the U.S. alone. An as-yet incurable neurological condition, MS occurs when the immune system attacks the protective sleeve surrounding nerve fibers and brain cells, known as a myelin sheath, resulting in an intractable breakdown of the nervous system.
Scientists have long suspected that MS is precipitated by an environmental trigger; likely some sort of microbial infection. Mouse models of MS are usually initiated in the lab by exposing animals to B. pertussis toxin, that is produced by the bacterium responsible for whooping cough, and one 2017 study found that gut microbiota taken from MS patients could directly result in MS in mice.
The question was which microbe to blame. While searching for an answer, Rumah stumbled across a 1986 study that highlighted an unexpected correlation: people living in areas with high sheep populations, such as Scotland and New Zealand, are more likely to suffer from MS.
Rumah thought of one potential culprit. "The bacteria C. perfringens, often found in sheep, makes over 20 different toxins," he says. "Its epsilon toxin has been known to break down the blood-brain barrier and cause MS-like symptoms in sheep." In the hopes of further exploring epsilon toxin as a possible environmental trigger for MS, Rumah joined Fischetti's lab in 2008.
The case for epsilon toxin
After several years, the team amassed substantial evidence that epsilon-toxin-producing C. perfringens are to blame.
Some of the earliest evidence came from mouse models. When Rumah and colleagues exposed mice to epsilon neurotoxin instead of the whooping cough, pertussis toxin, their blood-brain barrier broke down more dramatically and their nervous system lesions matched the telltale patterns seen in humans with MS. Then, with the help of PCR, the team demonstrated that humans with MS have much higher levels of epsilon-toxin-producing C. perfringens in their guts than the general population: 61 percent of MS patients tested positive, versus 13 percent of healthy controls and MS patients carried over 1000 times more of the bacterium in their gut than healthy, asymptomatic carriers.
As to how patients first become stabily colonized with this violent C. perfringens strain in the first place is unknown, "it is likely a genetic predisposition or the composition of their microbiome," Fischetti says. "We suspect that these particular strains colonize some people more effectively than others."
These findings have launched a search for therapeutics and diagnostics in the Fischetti lab for the early detection and treatment of MS—a direction that strikes to the heart of his lab's focus on finding unique ways of treating bacterial infections, particularly with antibiotic alternatives such as lysins. "There are very few organisms responsible for neurological diseases," he says. "Our lab focuses not only on infectious disease itself, but on how bacteria can initiate disease."
The team's immediate goal is to find definitive evidence linking epsilon toxin to MS. "We need to move from the gut and show that epsilon toxin is in the serum and cerebrospinal fluid of MS patients in the active phase of the disease," Rumah says. "If we can detect the toxin in the blood, then we'd have irrefutable evidence that this is at play in MS."
Comments
Post a Comment