Typhoid fever - Nature.com
Abstract
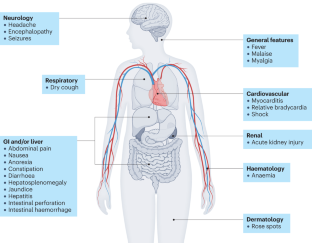
Typhoid fever is an invasive bacterial disease associated with bloodstream infection that causes a high burden of disease in Africa and Asia. Typhoid primarily affects individuals ranging from infants through to young adults. The causative organism, Salmonella enterica subsp. enterica serovar Typhi is transmitted via the faecal–oral route, crossing the intestinal epithelium and disseminating to systemic and intracellular sites, causing an undifferentiated febrile illness. Blood culture remains the practical reference standard for diagnosis of typhoid fever, where culture testing is available, but novel diagnostic modalities are an important priority under investigation. Since 2017, remarkable progress has been made in defining the global burden of both typhoid fever and antimicrobial resistance; in understanding disease pathogenesis and immunological protection through the use of controlled human infection; and in advancing effective vaccination programmes through strategic multipartner collaboration and targeted clinical trials in multiple high-incidence priority settings. This Primer thus offers a timely update of progress and perspective on future priorities for the global scientific community.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Rent or buy this article
Prices vary by article type
from$1.95
to$39.95
Prices may be subject to local taxes which are calculated during checkout

References
Dougan, G. & Baker, S. Salmonella enterica serovar Typhi and the pathogenesis of typhoid fever. Annu. Rev. Microbiol. 68, 317–336 (2014).
World Health Organization. Typhoid: vaccine preventable diseases surveillance standards. WHO https://www.who.int/publications/m/item/vaccine-preventable-diseases-surveillance-standards-typhoid (2018).
Basnyat, B., Qamar, F. N., Rupali, P., Ahmed, T. & Parry, C. M. Enteric fever. BMJ 372, n437 (2021).
Von Drigalski, K. W. Ueber Ergebnisse bei der Bekämpfung des Typhus nach Robert Koch [German]. Zentralbl. Bakteriol. 35, 776 (1904).
Kirchhelle, C., Pollard, A. J. & Vanderslott, S. Typhoid – from past to future. Clin. Infect. Dis. 69, S375–s376 (2019).
Ames, W. R. & Robins, M. Age and sex as factors in the development of the typhoid carrier state, and a method for estimating carrier prevalence. Am. J. Public. Health Nations Health 33, 221–230 (1943).
Antillon, M., Saad, N. J., Baker, S., Pollard, A. J. & Pitzer, V. E. The relationship between blood sample volume and diagnostic sensitivity of blood culture for typhoid and paratyphoid fever: a systematic review and meta-analysis. J. Infect. Dis. 218, S255–S267 (2018).
Nizamuddin, S., Khan, E. A., Chattaway, M. A. & Godbole, G. Case of carbapenem-resistant Salmonella Typhi infection, Pakistan, 2022. Emerg. Infect. Dis. J. 29, 2395–2397 (2023).
Phillips, M. T., Owers, K. A., Grenfell, B. T. & Pitzer, V. E. Changes in historical typhoid transmission across 16 U.S. cities, 1889-1931: quantifying the impact of investments in water and sewer infrastructures. PLoS Negl. Trop. Dis. 14, e0008048 (2020).
Vanderslott, S., Phillips, M. T., Pitzer, V. E. & Kirchhelle, C. Water and filth: reevaluating the first era of sanitary typhoid intervention (1840-1940). Clin. Infect. Dis. 69, S377–S384 (2019).
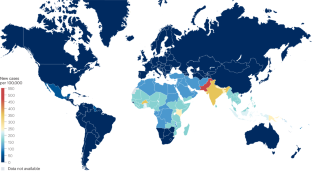
GBD 2017 Typhoid and Paratyphoid Collaborators The global burden of typhoid and paratyphoid fevers: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Infect. Dis. 19, 369–381 (2019).
Crump, J. A. Progress in typhoid fever epidemiology. Clin. Infect. Dis. 68, S4–S9 (2019).
Appiah, G. D. et al. Typhoid outbreaks, 1989-2018: implications for prevention and control. Am. J. Trop. Med. Hyg. 102, 1296–1305 (2020).
Reller et al. Presented at the 39th Annual Meeting of the Infectious Diseases Society of America (2022).
Mitscherlich, E. & Marth, E. H. Microbial survival in the environment (eds Mitscherlich, E. & Marth E.H.) 1–560 (Springer, 1984).
Cho, J.-C. & Kim, S. J. Viable, but non-culturable, state of a green fluorescence protein-tagged environmental isolate of Salmonella Typhi in groundwater and pond water. FEMS Microbiol. Lett. 170, 257–264 (1999).
Kingsley, R. A. et al. Functional analysis of Salmonella Typhi adaptation to survival in water. Env. Microbiol. 20, 4079–4090 (2018).
Andrews, J. R. et al. Environmental surveillance as a tool for identifying high-risk settings for typhoid transmission. Clin. Infect. Dis. 71, S71–S78 (2020).
Deen, J. et al. Community-acquired bacterial bloodstream infections in developing countries in south and southeast Asia: a systematic review. Lancet Infect. Dis. 12, 480–487 (2012).
Reddy, E. A., Shaw, A. V. & Crump, J. A. Community acquired bloodstream infections in Africa: a systematic review and meta-analysis. Lancet Infect. Dis. 10, 417–432 (2010).
Marchello, C. S., Dale, A. P., Pisharody, S., Rubach, M. P. & Crump, J. A. Prevalence of community-onset bloodstream infections among hospitalized patients in Africa and Asia: a systematic review and meta-analysis. Antimicrob. Agents Chemother. 64, e01974-19 (2019).
Garrett, D. O. et al. Incidence of typhoid and paratyphoid fever in Bangladesh, Nepal, and Pakistan: results of the Surveillance for Enteric Fever in Asia Project. Lancet Glob. Health 10, e978–e988 (2022).
Marks, F. et al. The Severe Typhoid in Africa Program: incidences of typhoid fever in Burkina Faso, Democratic Republic of Congo, Ethiopia, Ghana, Madagascar, and Nigeria. Preprint at https://ssrn.com/abstract=4292849 (2022).
Marks, F. et al. Incidence of invasive Salmonella disease in sub-Saharan Africa: a multicentre population-based surveillance study. Lancet Glob. Health 5, e310–e323 (2017).
Meiring, J. E. et al. Burden of enteric fever at three urban sites in Africa and Asia: a multicentre population-based study. Lancet Glob. Health 9, e1688–e1696 (2021).
John, J. et al. Burden of typhoid and paratyphoid fever in India. N. Engl. J. Med. 388, 1491–1500 (2023).
Crump, J. A., Luby, S. P. & Mintz, E. D. The global burden of typhoid fever. Bull. World Health Organ. 82, 346–353 (2004).
Antillón, M. et al. The burden of typhoid fever in low- and middle-income countries: a meta-regression approach. PLoS Negl. Trop. Dis. 11, e0005376 (2017).
Mogasale, V. et al. Burden of typhoid fever in low-income and middle-income countries: a systematic, literature-based update with risk-factor adjustment. Lancet Glob. Health 2, e570–e580 (2014).
Buckle, G. C., Walker, C. L. & Black, R. E. Typhoid fever and paratyphoid fever: systematic review to estimate global morbidity and mortality for 2010. J. Glob. Health 2, 10401 (2012).
Institute of Health Metrics and Evaluation. Global incidence of typhoid fever. IHME https://vizhub.healthdata.org/gbd-compare/ (2019).
Crump, J. A. & Kirk, M. D. Estimating the burden of febrile illnesses. PLoS Negl. Trop. Dis. 9, e0004040 (2015).
Marchello, C. S., Hong, C. Y. & Crump, J. A. Global typhoid fever incidence: a systematic review and meta-analysis. Clin. Infect. Dis. 68, S105–S116 (2019).
Crump, J. A. et al. Estimating the incidence of typhoid fever and other febrile illnesses in developing countries. Emerg. Infect. Dis. 9, 539–544 (2003).
Marchello, C. S., Birkhold, M. & Crump, J. A. Complications and mortality of typhoid fever: a global systematic review and meta-analysis. J. Infect. 81, 902–910 (2020).
Gibani, M. M. et al. Homologous and heterologous re-challenge with Salmonella Typhi and Salmonella Paratyphi A in a randomised controlled human infection model. PLoS Negl. Trop. Dis. 14, e0008783 (2020).
Im, J. et al. Protection conferred by typhoid fever against recurrent typhoid fever in urban Kolkata. PLoS Negl. Trop. Dis. 14, e0008530 (2020).
Brockett, S. et al. Associations among water, sanitation, and hygiene, and food exposures and typhoid fever in case-control studies: a systematic review and meta-analysis. Am. J. Trop. Med. Hyg. 103, 1020–1031 (2020).
Tadesse, B. T. et al. Prevention of typhoid by Vi conjugate vaccine and achievable improvements in household water, sanitation, and hygiene: evidence from a cluster-randomized trial in Dhaka, Bangladesh. Clin. Infect. Dis. 75, 1681–1687 (2022).
Gunn, J. S. et al. Salmonella chronic carriage: epidemiology, diagnosis, and gallbladder persistence. Trends Microbiol. 22, 648–655 (2014).
Dunstan, S. J. et al. Variation at HLA-DRB1 is associated with resistance to enteric fever. Nat. Genet. 46, 1333–1336 (2014).
Saad, N. J. et al. Seasonal dynamics of typhoid and paratyphoid fever. Sci. Rep. 8, 6870 (2018).
Thindwa, D., Chipeta, M. G., Henrion, M. Y. R. & Gordon, M. A. Distinct climate influences on the risk of typhoid compared to invasive non-typhoid Salmonella disease in Blantyre, Malawi. Sci. Rep. 9, 20310 (2019).
Levy, K., Smith, S. M. & Carlton, E. J. Climate change impacts on waterborne diseases: moving toward designing interventions. Curr. Env. Health Rep. 5, 272–282 (2018).
Gao, Q. et al. Impact of temperature and rainfall on typhoid/paratyphoid fever in Taizhou, China: effect estimation and vulnerable group identification. Am. J. Trop. Med. Hyg. 106, 532–542 (2021).
Hickman-Brenner, F. W. & Farmer, J. J. III Bacteriophage types of Salmonella typhi in the United States from 1974 through 1981. J. Clin. Microbiol. 17, 172–174 (1983).
Chattaway, M. A., Langridge, G. C. & Wain, J. Salmonella nomenclature in the genomic era: a time for change. Sci. Rep. 11, 7494 (2021).
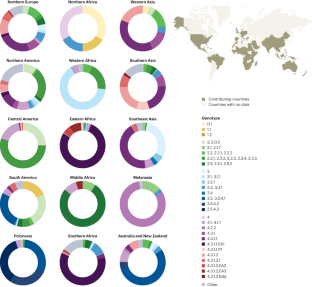
Wong, V. K. et al. Phylogeographical analysis of the dominant multidrug-resistant H58 clade of Salmonella Typhi identifies inter- and intracontinental transmission events. Nat. Genet. 47, 632–639 (2015).
Tanmoy, A. M. et al. Paratype: a genotyping tool for Salmonella Paratyphi A reveals its global genomic diversity. Nat. Commun. 13, 7912 (2022).
Kariuki, S. et al. Multiple introductions of multidrug-resistant typhoid associated with acute infection and asymptomatic carriage, Kenya. Elife 10, e67852 (2021).
Dyson, Z. A. et al. Genomic epidemiology and antimicrobial resistance transmission of Salmonella Typhi and Paratyphi A at three urban sites in Africa and Asia. Preprint at medRxiv https://doi.org/10.1101/2023.03.11.23286741 (2023).
Wong, V. K. et al. An extended genotyping framework for Salmonella enterica serovar Typhi, the cause of human typhoid. Nat. Commun. 7, 12827 (2016).
Dyson, Z. A. & Holt, K. E. Five years of GenoTyphi: updates to the Global Salmonella Typhi Genotyping Framework. J. Infect. Dis. 224, S775–S780 (2021).
Carey, M. E. et al. Global diversity and antimicrobial resistance of typhoid fever pathogens: insights from a meta-analysis of 13,000 Salmonella Typhi genomes. eLife 12, e85867 (2023).
da Silva, K. E. et al. The international and intercontinental spread and expansion of antimicrobial-resistant Salmonella Typhi: a genomic epidemiology study. Lancet Microbe 3, e567–e577 (2022).
Comments
Post a Comment