How to Avoid the Dreaded Norovirus - Scientific American
Norovirus, the infamous "winter vomiting disease" that has people keeling over on the toilet with a bad case of the runs, is making its seasonal rampage through countries that include the U.S., the U.K. and Canada. Impervious to hand sanitizers and able to remain infectious outside the body for weeks, the notoriously unpleasant gastrointestinal virus can strike any time of year, but cases tend to peak in the Northern Hemisphere between November and April.
"It's one of the many viruses that affects our GI tract, but it's the leading cause of vomiting and diarrhea from acute gastroenteritis in all ages in the United States," says Christopher Cao, an assistant professor of gastroenterology at the Icahn School of Medicine at Mount Sinai in New York City. "So it causes a whole lot of infection."
As of early March, U.K. Health Security Agency data show cases are more than double the five-season average prior to the pandemic. Agency officials have said levels "are currently the highest we have seen at this time of year in over a decade." According to the U.S. Centers for Disease Control and Prevention, an average of 16.3 percent of norovirus PCR tests were positive as of March 4, 2023, compared with 14.6 percent on March 5, 2022. The CDC says the total number of outbreaks so far during the 2022–2023 season is still within the range of past norovirus seasons. But the national numbers may not reflect what's happening in states that do not participate in the CDC's norovirus reporting.
"While I think that there is a pretty good trend that overall, throughout the country, the number of norovirus outbreaks have not really increased, I don't think it's completely representative of all the different communities in the U.S.," Cao says. "Anecdotally, I've seen a lot of norovirus in New York [City] recently in my patients, and that may not necessarily be reflected in the data that the CDC is providing because they don't collect data from New York [State]." The available New York City Health Department data do not specify norovirus as a culprit but do show a recent increase in emergency room visits for vomiting or diarrhea.
Other health experts also have a hunch that norovirus is behind this trend. The virus is suspected to have sickened more than 100 students at a Phoenix elementary school and has prompted a school closure in Livonia, Mich., a suburb of Detroit. The states whose health departments participate in the CDC's norovirus tracking program are Alabama, Massachusetts, Michigan, Minnesota, Nebraska, New Mexico, North Carolina, Ohio, Oregon, South Carolina, Tennessee, Virginia, Wisconsin and Wyoming.
What gives this persistent pathogen its superpowers? And is there any hope of dodging it amid a possible outbreak? Scientific American spoke to some experts about this year's situation.
What are the symptoms of norovirus, and who is most at risk of severe illness?
The virus commonly causes profuse diarrhea and vomiting, along with nausea and stomach cramps. Symptoms begin about 12 to 48 hours after exposure and usually last roughly one to three days.
"People who've had it a lot of time will just sleep on the floor of the bathroom because they're going a lot," says Melissa Jones, a virologist and an assistant professor of microbiology and cell science at the University of Florida. "It's pretty miserable. Most people recover but are pretty dehydrated for a couple days."
Norovirus targets the cells that line the small intestine, but not much is known about how it attacks the body so profoundly in such a short time. "They cause hundreds of millions of infections worldwide every year, but we actually know relatively little about how the virus actually does it," says Jones, who is currently investigating if interactions with the gut microbiome might aid norovirus's pathogenicity, which is the case for poliovirus.
Norovirus sickens 19 million to 21 million people in the U.S. each year, according to the CDC. Most people recover quickly, but severe cases—particularly among children under age five, adults age 85 or older and the immunocompromised—can lead to hospitalization and sometimes death. Globally it contributes to an estimated 50,000 infant fatalities per year, mostly in developing countries. Fevers are rare with norovirus, Jones says, but immunocompromised people can develop them and have other prolonged symptoms. In very rare cases, norovirus infection can persist in immunocompromised individuals for weeks or years.
How does it spread?
Norovirus outbreaks can spread rapidly in confined spaces such as day care centers, schools, college dorms and health care facilities. Cruise ships' close living quarters and shared spaces are often associated with norovirus, but the CDC notes that the link might be a result of cases often being tracked more frequently on cruise ships than in other places.
Infection usually starts with someone ingesting just a few microscopic particles of an infected person's feces or vomit. The virus often spreads when people consume contaminated or mishandled food. The CDC blames norovirus for about half of all U.S. food-related illness outbreaks. Oysters and other filter-feeding shellfish, along with salads and produce, are commonly involved in outbreaks, Cao says. Some experts estimate that as few as 10 viral particles can cause illness.
"Within about 18 hours of consumption, you start to have symptoms, and you just produce massive amounts of virus," Jones says. "You're talking, like, about a billion virus particles per gram of stool. And you're going to the bathroom all the time. That's a lot that's coming out of somebody."
What can be done to prevent or slow down transmission?
Norovirus is often colloquially called a "24-hour stomach bug" or "stomach flu," but Cao notes that it's not an influenza virus. As a member of the Caliciviridae family, it is a single-stranded RNA virus that doesn't rely on an exterior "envelope" for protection. This makes it particularly resilient and evasive.
"Being nonenveloped is really important because that means that it's resistant to alcohol," says Patricia Foster, a professor emerita of biology at Indiana University Bloomington, who has studied norovirus. Alcohol-based products such as hand sanitizers work by disrupting the membranes that envelop many viruses such as influenza and the COVID-causing virus SARS-CoV-2—so such products are ineffective against norovirus, Foster says.
Notably, norovirus can survive for up to two weeks on surfaces. In contrast, SARS-CoV-2 only does so for a few hours or days. And norovirus can remain infectious in water for two months or more.
Your best line of defense is to wash your hands—a lot.
Symptoms may stop after a couple of days, but infected people can continue to shed the virus in their stool for a few weeks, Jones says. So for the sake of others, keep washing up thoroughly with soap and water, even after you feel better.
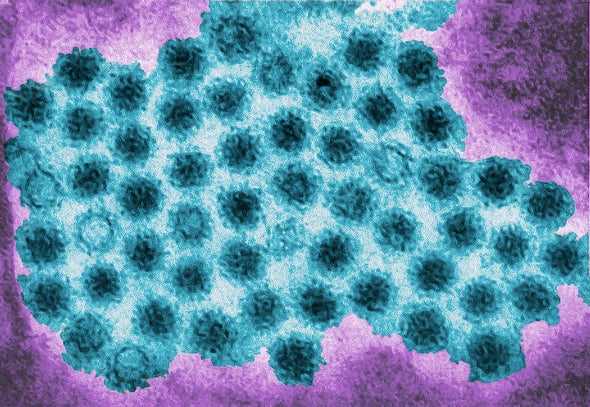
The virus's genetic material is also surrounded by a tightly bound protein shell, or capsid, which Foster says may explain its incredible resistance to temperature and acidity. Studies show norovirus can withstand up to 140 degrees Fahrenheit and can still be infectious at freezing temperatures. Scientists have linked norovirus's cold tolerance, along with more people being indoors in close quarters, to its prevalence in winter. But Jones says it's still not fully understood why norovirus tends to take off in the colder months.
"It's a very hardy virus, and so it really does require a lot of care and effort into preventing that spread," Cao says. "A lot of the standard cleaning agents won't work very well on norovirus. So certain bleach solutions are actually recommended to clean norovirus off surfaces."
Places such as schools, hospitals or long-term care facilities might consider temporarily closing certain communal spaces and thoroughly cleaning them. U.S. schools aren't required to close for norovirus outbreaks, but many have their own policies that require shutting down the entire campus for cleaning if cases are high despite other control measures—such as removing infected students or staff from campus, using personal protective equipment and quickly disinfecting surfaces after vomiting episodes.
How is norovirus treated?
If prevention measures fail, Cao says the best thing an infected person can do is to stay at home and stay hydrated. There is no cure, but symptoms usually resolve on their own. If symptoms persist more than three days, people should seek medical care, especially if they are immunocompromised, very young or elderly, Cao says. He adds that fevers and bloody diarrhea are other potential signs of trouble.
"We don't see [severe seasons of] norovirus every single year, but having really huge outbreaks is usually the result of evolution" of the virus, Jones explains. "We get a new strain that crops up where we don't have a lot of immunity, and so we get a huge spike in disease because this new strain is making its way around." Like other single-stranded RNA viruses, norovirus has a high mutation rate. This promotes genetic diversity, so new variants "pop up all the time," Foster says.
Emerging variants also pose a challenge in developing a norovirus vaccine. As with COVID and flu, new vaccine formulas would need to be developed and administered regularly as variants show up. Another barrier to vaccine development has been the difficulty of cultivating the virus in cell cultures and testing in an animal model that would exhibit the same disease seen in humans. Several companies, such as HilleVax and Vaxart, are working on possibilities that have undergone initial clinical trials, including an oral vaccine.
"I know that over the past three years we've really focused on respiratory viruses like coronavirus, where we are very mindful to wear masks [and] to wash your hands sometimes with alcohol-based sanitizers," Cao says. "But I think we do also have to remember that there are other types of viruses that transmit differently."
Comments
Post a Comment