Disseminated nocardiosis in a patient with alcoholic liver cirrhosis: a ... - BMC Infectious Diseases
The patient was a 47-year-old man with a history of heavy alcohol intake over the past 4 years (3–4 drinks per day), which was complicated by alcoholic liver cirrhosis (Child–Pugh C/MELD 22), portal hypertension, and esophageal varices grade 2. He presented to our emergency department with redness and swelling in the left eye for 2 months and bilateral diminished vision, mainly in the left eye, over the previous month. The patient had no history of ocular trauma. The associated symptoms included mild right upper quadrant pain, jaundice, unintentional weight loss (approximately 22 kg in the past 3 months), pruritus, and dark-colored urine. Ophthalmic examination done upon presentation is shown in (Table 1).
The initial blood analysis was as follows: complete blood count: white blood cells: 10.3 × 103/µL (normal range 4.5 to 11.0 × 106/μL), red blood cells: 3.5 × 106/μL (normal range 4.7 to 6.1 × 106/μL), hemoglobin: 11.2 g/ldl (normal range 13.2 to 16.6 g/dl), platelets: 225 × 103/µL (normal range 150 to 400 × 103/µL); creatinine: 64 µmol/L (normal range 53 to 97.2 µmol/L), serum sodium: 131 mmol/L (normal range 136 and 145 mmol/L), serum potassium: 4.4 mmol/L (normal range 3.6 to 5.2 mmol/L), serum magnesium: 0.74 mmol/L (normal range 0.85 to 1.10 mmol/L), corrected calcium: 2.2 mmol/L (normal range 2.2 to 2.7 mmol/L), Erythrocyte sedimentation rate: 95 mm/hr (normal range 0 to 15 mm/hr); C-reactive protein level: 92 mg/L (normal range < 3 mg/L); total bilirubin: 132 µmol/L (normal range 1.71 to 20.5 µmol/L); alkaline phosphatase: 151 U/L (normal range 44 to 147 U/L); alanine aminotransferase: 33 U/L (normal range 4 to 36 U/L); albumin: 28.7 g/L (normal range 34 to 54 g/L); and lactic acid: 1.8 mmol/L (normal range 0.5 to 2.2 mmol/L).
Computed tomography (CT) of the brain and orbits revealed two ring-enhancing lesions in the left frontal lobe along with orbital findings suggestive of left orbital endophthalmitis (Fig. 1). Contrast-enhanced magnetic resonance imaging was performed to confirm the diagnosis of supra- and infratentorial brain abscesses and left eye endophthalmitis with a subretinal abscess (Fig. 2).
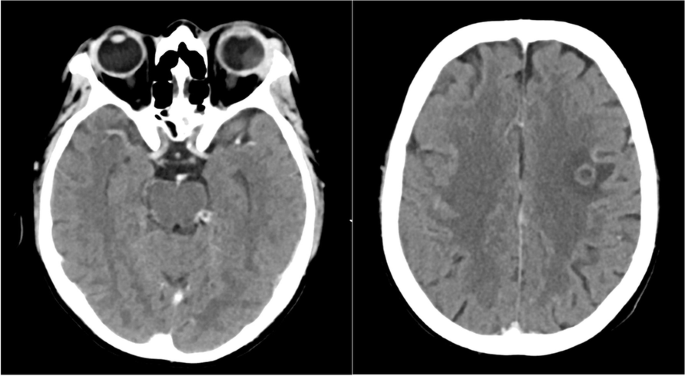
Left image: Axial contrast-enhanced CT scan of the orbits showing generalized scleral thickness of the left eye with heterogeneous increase in density of the vitreous content. Also seen is soft tissue swelling, orbital proptosis, peri- and post-septal orbital fat stranding plus thickening, and enhancement of the globe wall. Findings that are suggestive of endophthalmitis and subretinal abscess. Enlargement of the lacrimal gland is also noted. Right image: Axial section of a contrast-enhanced CT of the brain shows a ring- enhancing lesion in the left frontal lobe measuring 0.9 cm with surrounding vasogenic edema. Findings consistent with intraparenchymal abscess
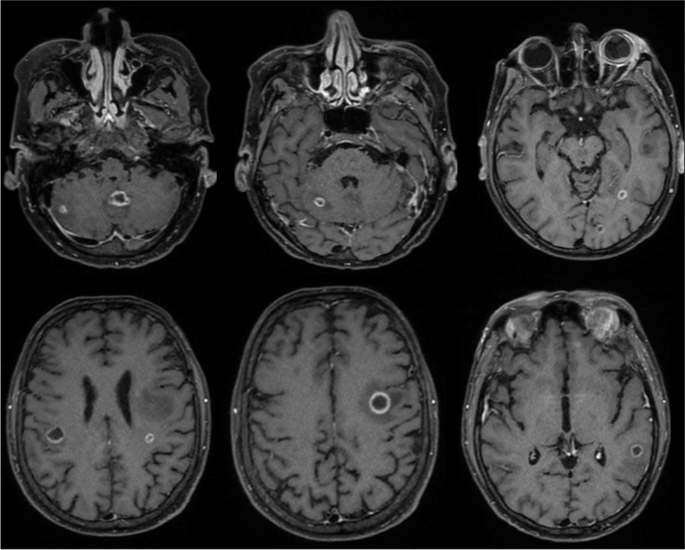
Contrast-enhanced T1-weighted images. Multiple supra- and infratentorial rim-enhancing lesions. Also noted surrounding vasogenic edema. Findings that are consistent with abscesses. Images on the right show enhancement of the left globe and surrounding soft tissue. Relatively hyperintense subretinal fluid is noted. Findings that are consistent with left eye endophthalmitis and subretinal abscess. The right orbit shows enhancement of the extra-conal soft tissue suggesting involvement
Magnetic resonance cholangiopancreatography was performed to rule out malignancy and hepatic lesions; however, it only showed a cirrhotic liver with portal hypertension without any focal lesions. However, an incidental finding of bilateral lower-lobe pulmonary nodules was noted, for which a dedicated chest CT was planned.
High-resolution chest CT revealed multiple small bilateral cystic and cavitary lung lesions (Fig. 3).
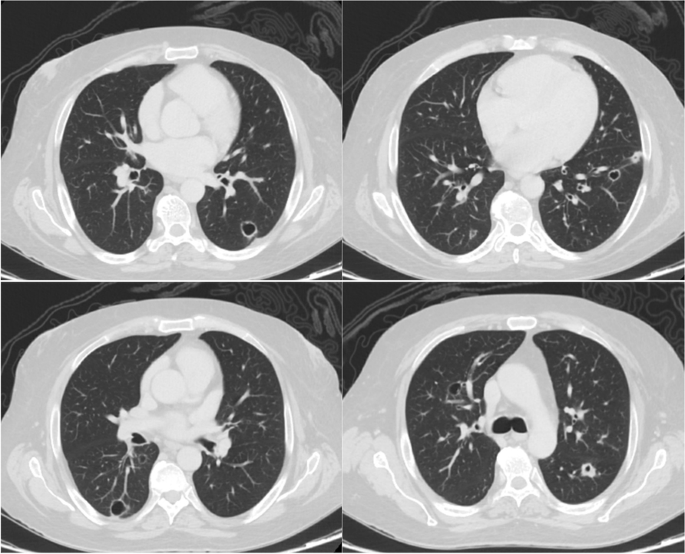
Axial sections of a contrast-enhanced CT scan of the chest show multiple bilateral cystic and cavitary lung lesions, predominantly involving the lower lobes. A cavitary nodule is seen in the superior segment of the left lower lobe showing thickened wall (upper left image)
The patient underwent further investigations, including blood culture, bronchoalveolar lavage culture, AFB of three samples from saliva, QuantiFERON TB gold test, HIV tests, and syphilis serology. However, all tests had negative results.
An ophthalmic examination shown in (Table 1) revealed a subretinal abscess in the right eye. The patient was initially suspected to have endogenous endophthalmitis and was started on intravitreal vancomycin, ceftazidime, and voriconazole. A few days later, the patient's left eye failed to improve, and as a result, evisceration of the left eye was decided.
Microbiological studies were performed on the left eye specimen; Ziehl–Neelsen (ZN) staining was negative; however, the modified ZN stain was positive. Partial acid-fast bacteria (AFB) stained positive.
Culture of the left eye swab done in Blood agar and MacConkey agar confirmed the diagnosis of Nocardia farcinica infection. Identification was performed using MALDI-TOF and sensitivity using the manual E-test (Table 2).
Histopathological examination revealed dense histiocytic and neutrophilic infiltrates consistent with an abscess (acute endophthalmitis). Special staining including Grocott's methenamine silver, and periodic acid-Schiff staining yielded negative results, while Acid-fast bacteria (AFB) satin was partially positive.
When disseminated nocardiosis was confirmed, the patient was started on Nocardia treatment (imipenem 500 mg every 8 h IV, trimethoprim/sulfamethoxazole 255 mg every 6 h, and amikacin 15 mg/kg once daily). Within a few days, the patient's condition improved with complete resolution of the subretinal abscess in the right eye. Follow-up ophthalmic examination during treatment is shown in (Table 3).
Follow-up magnetic resonance imaging of the brain also showed interval regression in the size of multiple peripherally located bilateral ring-enhancing lesions. However, CT angiography of the chest, which was performed to rule out pulmonary embolism a month after the previous chest CT, revealed progression of multiple bilateral cavitary lung lesions with the development of pneumomediastinum (Fig. 4).
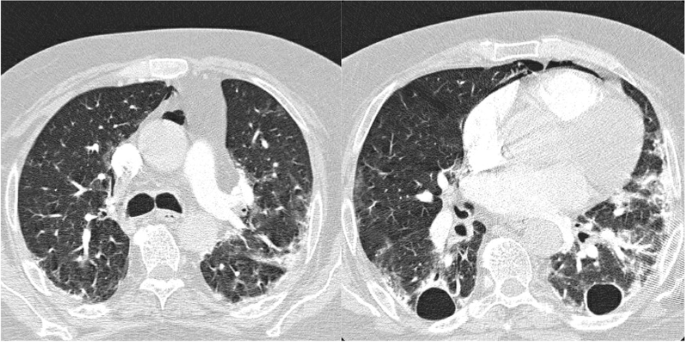
Axial sections of CT angiography of the pulmonary arteries, performed a month after the previous chest CT (Fig. 3), show progression of bilateral cavitary lung lesions and more evident traction bronchiectasis. It also shows development of bilateral peripheral patchy ground glass opacities and compressive atelectasis. Note is also made of pneumomediastinum
During hospital stay, the patient developed acute pancreatitis and acute kidney injury, which were primarily treated with hydration and pain management.
The patient received imipenem, amikacin, trimethoprim/sulfamethoxazole, and neomycin for 6 weeks. The patient was maintained on ocular prednisolone and cyclopentolate, as recommended by an ophthalmologist.
The patient's hospital course was complicated by his aggressive and advanced condition. He developed septic shock and died of cardiac arrest in the intensive care unit.
Comments
Post a Comment