A case report of a brain abscess due to prevotella oris and a review ... - BMC Infectious Diseases
A 63-year-old male patient presented with pain in the right frontotemporal region accompanied by fever with a maximum temperature of 39 °C 15 days prior to admission; he had intermittent diplopia shortly after admission; and, 5 days prior to admission, he had showed unresponsiveness. There was no previous history of infections, surgery or trauma.
At the time of consultation, his vital signs were stable, and his cardiopulmonary and abdominal investigations were normal. The neurologic examination showed a somnolent state, with the patient answering off the point, and he had dysarthria. The cranial nerve examination was normal, but neck rigidity, weakened muscles of the limbs and positive Kernig's sign on the left side were noted. A brain MRI was performed and revealed abnormal signals in the bilateral basal ganglia, bilateral periventricular and corpus callosum; abnormal signals and enhancement changes in the sellar region, superior sellar region and left medial temporal region; abnormal signal enhancement in the anterior longitudinal fissure and ventral brainstem; and inflammatory signals in the right ethmoid and sphenoid sinuses (Fig. 1A-F). Routine laboratory studies showed mostly normal findings, with the exception of slightly elevated D-dimer level and ESR. Cerebrospinal fluid (CSF) analysis showed the following: pressure 210 mmH2O, leukocyte count 250*106/L (72% polymorphonuclear, 28% monocytes) without altered erythrocytes, protein 1.10 g/l and glucose 2.99 mmol/l, and the CSF was absent for oligoclonal bands. Cytological examination of the CSF showed no malignant cells. CSF cultures were negative for bacteria, fungi, and mycobacteria, and polymerase chain reaction to test for herpes simplex virus (HSV PCR) was negative.
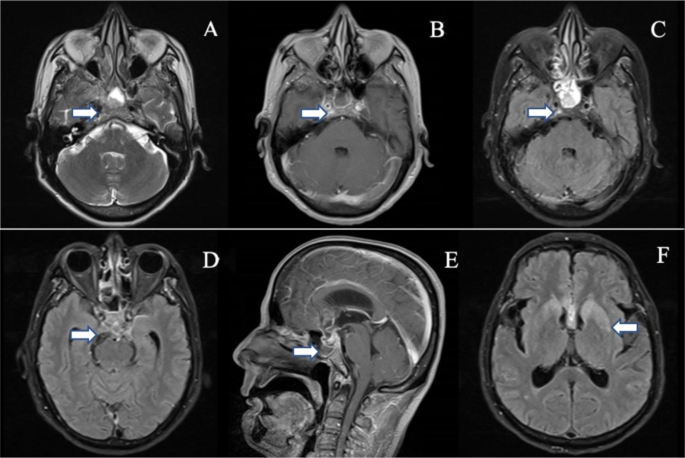
MRI of the brain: A: Slice of irregular and slightly long T2 signal in the sellar area. B, C: Slice of irregular enhancement changes in the sellar region. D: High signal in the flair sequence in the saddle region. E: Slice of irregular enhancement changes in the sellar and suprasellar regions. F: High signal in the flair sequence in the bilateral basal ganglia regions
The patient was treated empirically with intravenous levofloxacin and piperacillin-tazobactam for 7 days before being referred, but no significant efficacy was seen. Based on the cerebrospinal fluid analysis and the lack of treatment efficacy, the diagnosis of intracranial abscess was considered, and anti-infective treatment with vancomycin, meropenem, and ganciclovir was given for 5 days. The patient's symptoms did not improve with these treatments. We performed next-generation sequencing, which showed positive results, mainly Prevotella oris, with 1328 sequences detected and a relative abundance of 49. 94%, and a small number of Peptostreptococcus stomatis, with 290 sequences detected and a relative abundance of 11. 13%. When the results of this testing became available, the vancomycin treatment was discontinued, and the patient was maintained on ceftriaxone and metronidazole.
Further investigations were performed to determine the source of the infection. We noted that brain MRI suggested inflammatory signals in the right septal and pterygoid sinuses. Nasal endoscopy revealed a purulent discharge visible in the right pterygoid sinus orifice (Fig. 2A-B), which also revealed Prevotella oris. Based on this finding, the revealed anaerobic bacteria could be logically responsible for a contiguous spread of infection following nasosinusitis.
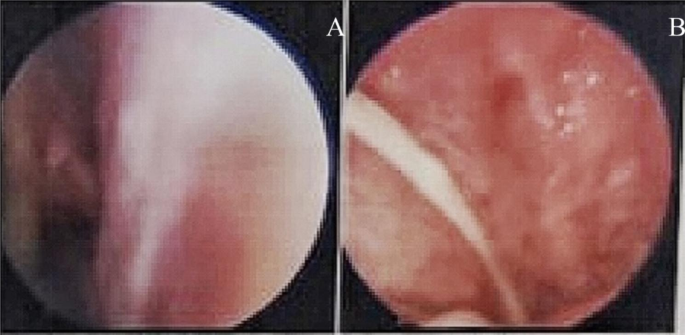
Nasal endoscopy showing an outflow of pus from the right sphenoid sinus ostium
After 14 days of treatment, the patient's symptoms were significantly improved, his consciousness was clear, and he could communicate normally. However, shortly after the symptoms improved, his condition worsened again, and he fell into a shallow coma and had speechlessness. Brain CT showed dilatation of the supratentorial ventricular system and widening of the sulcioencephalic fissure (Fig. 3A-B). We thought this was caused by hydrocephalus complicated by an intracranial abscess, so we transferred the patient to the neurosurgery department for ventriculoperitoneal shunting. After the operation, ceftriaxone and metronidazole were continued for 4 weeks, and the patient gradually recovered to his premorbid state and was soon discharged from the hospital. During the later follow-up process, we learned that he no longer had these symptoms.
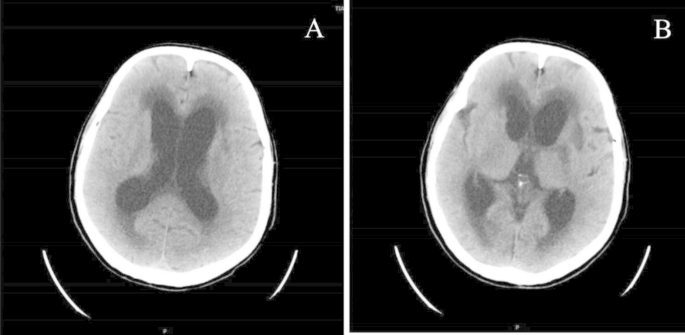
CT of the brain: dilatation of the supratentorial ventricular system and widening of the sulcioencephalic fissure
Comments
Post a Comment