Antibiotic-Resistant Biofilms Eliminated by “Living Medicine” - Genetic Engineering & Biotechnology News
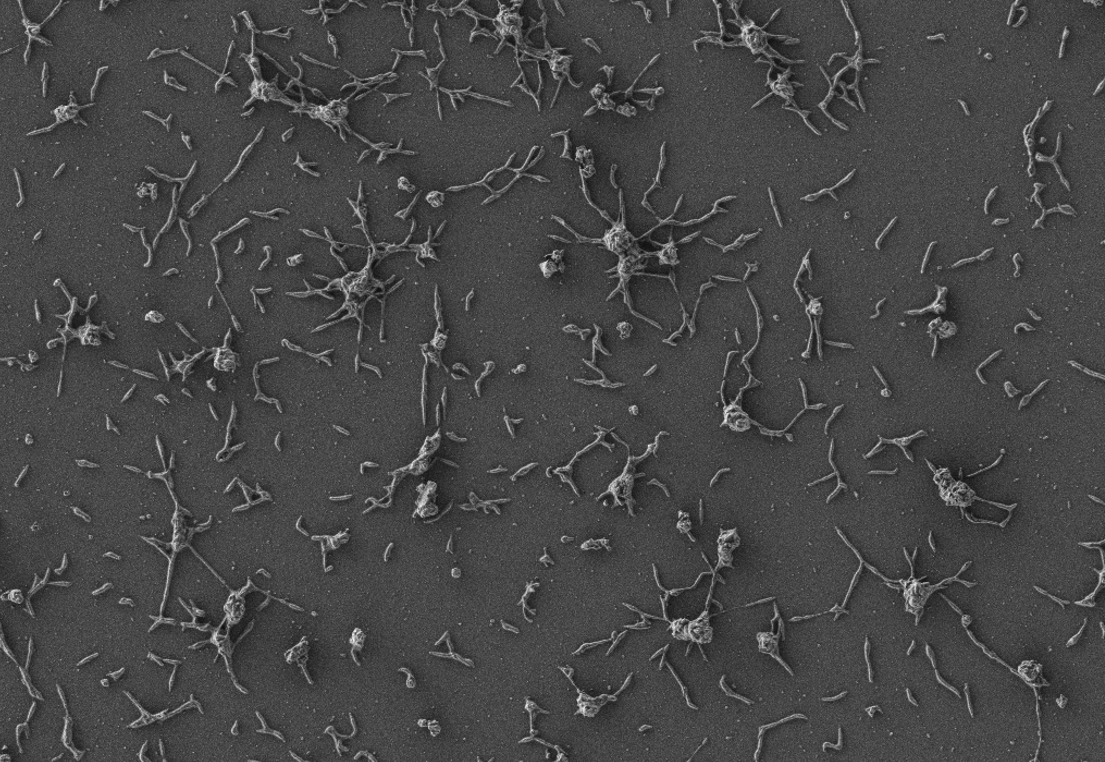
Bacteria that grow on medical implants have a siege mentality. They form biofilms, which function rather like castle walls. To undermine these walls, scientists have engineered a bacterium that produces and secretes enzymes that dissolve biofilm structures and kill biofilm bacteria. Once the engineered bacterium is injected near an infection site, it works like a microscopic sapper, breaking down defenses that would fend off antibiotics and elements of the immune system.
The scientists, who are affiliated with the Centre for Genomic Regulation (CRG) and Pulmobiotics, made a sapper out of Mycoplasma pneumoniae. Ordinarily, this bacterium is a human lung pathogen. However, it has attributes that make it a suitable recruit. It has a unique genetic code, which reduces the likelihood of gene transfer, and it lacks a cell wall, which allows it to express proteins that target peptidoglycans of pathogenic bacteria.
To ready M. pneumoniae for combat, the scientists stripped down the bacterium's genome, removing its ability to cause disease. Then the scientists modified the genome to enhance the bacterium's ability to secrete expressed factors, which, thanks to additional genome modification, included antibiofilm factors. Altogether, the modifications resulted in a "living medicine."
The scientists tested their living medicine's ability to treat Staphylococcus aureus–infected catheters in vitro, ex vivo, and in vivo. According to the scientists, the living medicine eliminated infections in all three scenarios. In addition, injecting the therapy under the skin of mice treated infections in 82% of the treated animals.
Detailed results appeared in the journal Molecular Systems Biology, in a paper titled, "Engineering a genome-reduced bacterium to eliminate Staphylococcus aureus biofilms in vivo." In this paper, the scientists expressed optimism that living therapeutics could be developed that would eliminate the infections that grown on medical implants such as catheters, pacemakers, and prosthetic joints. These infections are highly resistant to antibiotics and account for 80% of all infections acquired in hospital settings.
"We first determined that removal of the pathogenic factors fully attenuated the chassis strain in vivo," the article's authors wrote. "We then designed synthetic promoters and identified an endogenous peptide signal sequence that, when fused to heterologous proteins, promotes efficient secretion. Based on this, we equipped the chassis strain with a genetic platform designed to secrete antibiofilm and bactericidal enzymes, resulting in a strain capable of dissolving Staphylococcus aureus biofilms."
The new treatment specifically targets biofilms, colonies of bacterial cells that stick together on a surface. The surfaces of medical implants are ideal growing conditions for biofilms, where they form impenetrable structures that prevent antibiotics or the human immune system from destroying the bacteria embedded within. Biofilm-associated bacteria can be a thousand times more resistant to antibiotics than free-floating bacteria.
S. aureus is one of the most common species of biofilm-associated bacteria. S. aureus infections do not respond to conventional antibiotics, requiring patients to surgically remove any infected medical implants. Alternative therapies include the use of antibodies or enzymes, but these are broad-spectrum treatments that are highly toxic for normal tissues and cells, causing undesired side effects.
The authors of the study hypothesized that introducing living organisms that directly produce enzymes in the local vicinity of biofilms is a safer and cheaper way of treating infections. Bacteria are an ideal vector, as they have small genomes that can be modified using simple genetic manipulation.
The researchers' immediate goal is to use the modified bacteria to treat biofilms building around breathing tubes, as M. pneumoniae is naturally adapted to the lung.
"Our technology, based on synthetic biology and live biotherapeutics, has been designed to meet all safety and efficacy standards for application in the lung, with respiratory diseases being one of the first targets," said María Lluch, PhD, co-corresponding author of the study and CSO of Pulmobiotics. "Our next challenge is to address high-scale production and manufacturing, and we expect to start clinical trials in 2023."
The modified bacteria may also have long-term applications for other diseases. "Bacteria are ideal vehicles for 'living medicine' because they can carry any given therapeutic protein to treat the source of a disease," noted ICREA research professor Luis Serrano, PhD, director of the CRG and co-author of the study. "One of the great benefits of the technology is that once they reach their destination, bacterial vectors offer continuous and localized production of the therapeutic molecule. Like any vehicle, our bacteria can be modified with different payloads that target different diseases, with potentially more applications in the future."
Comments
Post a Comment