Mpox and primary syphilis co‐infection in a newly arrived traveller ... - The Medical Journal of Australia
Clinical record
A 27‐year‐old male South American traveller developed painful genital ulcers accompanied by fever and right‐sided groin pain on arrival in Sydney and consulted a general practitioner. Testing showed reactive Treponema pallidum IgG (TPA), T. pallidum particle agglutination (TPPA), fluorescent treponemal antibody (FTA) and rapid plasma reagin (RPR) of 1:8. He was negative for human immunodeficiency virus infection. He was referred immediately to our sexual health clinic where he gave a history of past syphilis in 2020 (treated adequately) and non‐reactive RPR in the previous six months. Last sexual contact was three weeks prior in South America with a male and female couple. He had unprotected oral sex (giving and receiving with both partners) and protected vaginal intercourse. There was no anal sex.
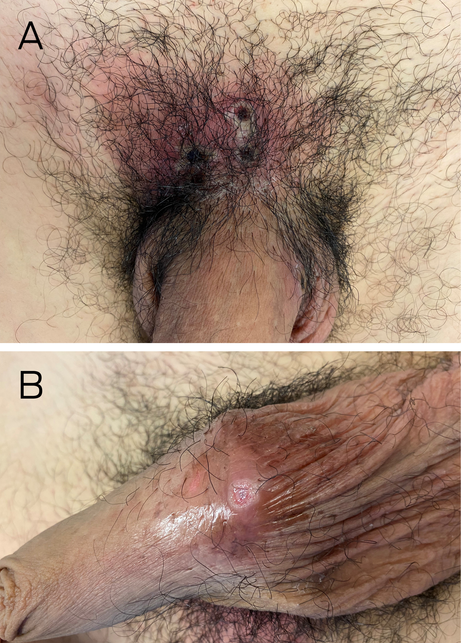
On examination, two distinct types of ulcers were noted in the genital area. A cluster of four painful superficial ulcers were seen in the pubic area, of about 1 cm diameter each with yellow slough under thick black scabs and surrounding erythema (cellulitis; Box, A). A separate single painless indurated ulcer was seen on the underside of the penis at the penoscrotal junction (clean healing base and no surrounding erythema), suggestive of a chancre (Box, B). A painful new vesicle was seen on the dorsum of his left ankle. A right inguinal lymph node was enlarged and tender. He reported fever, headache and myalgia.
Dual pathology was clinically suspected and samples for monkeypox virus (MPXV) DNA (dry scab in sterile urine jar and ulcer swab) and syphilis DNA (separate swabs from necrotic ulcers and single painless ulcer) were collected. He was treated presumptively with intramuscular benzathine penicillin 2.4 million units for primary syphilis, oral amoxicillin/clavulanic acid for cellulitis, and paracetamol for pain. He was advised to isolate pending results. Eight hours later, swabs from the painful ulcers and dry scabs returned positive for MPXV DNA and he was further advised to isolate for 21 days or until lesions were healed with regrowth of normal skin (whichever is longer). Neither syphilis DNA nor MPXV DNA was detected from the suspected chancre, possibly due to its healed base. This single ulcer may have preceded the pubic cluster, unnoticed due to position and painlessness or it may have been an atypical or evolving mpox (formerly monkeypox) ulcer. All ulcer swabs using our multiplex genital ulcer DNA panel tested negative for herpes simplex virus 1 and 2, lymphogranuloma venereum, varicella zoster virus, cytomegalovirus, and Haemophilus ducreyi.
Our social worker provided written information in Spanish and liaised with the local public health unit for contact tracing. Two household contacts were given mpox vaccines (Jynneos, Bavarian Nordic) within 24 hours. There were no sexual contacts in Australia. Hotel accommodation was provided for isolation with phone follow‐up. The ulcers and cellulitis improved markedly over ten days and he was released from isolation three weeks after symptom onset when all lesions were healed. According to current guidelines, he was advised to use condoms for sexual intercourse for a further eight weeks.1
Discussion
The first case of mpox in Australia was reported in May 2022, diagnosed in a man returned from overseas.2 Since then, there have been 145 cases in Australia as of 5 June 2023, mostly acquired overseas.3 An international case series published in August 2022 described 528 infections reported from 27 April to 24 June 2022 in 43 sites in 16 countries.4 It found that 98% of infections were in gay and bisexual men and 95% were through sexual transmission. Twenty‐nine per cent of patients in this study also had a sexually transmitted infection diagnosed at the same time, most commonly syphilis (9%). Skin lesions were commonest in the anogenital area (73%), predominantly vesiculopustular ulcers. Single genital ulcer presentation of mpox was not uncommon, highlighting the possibility of misdiagnosis with syphilis in particular.
Worldwide, syphilis rates have increased in the past decade. The World Health Organization reports an average of 11.8% of men who have sex with men were infected with syphilis in 2019 in 25 reporting countries.5 The incidence of syphilis has risen in Australia since 2011, and the latest National Syphilis Surveillance quarterly report shows that 83% of infectious syphilis notifications in major cities were in non‐Indigenous men (reporting period 1 April 2021 to 31 March 2022).6
We present a case of atypical genital ulceration in a bisexual man with recent travel history. Dual pathology was suspected due to two distinct ulcer types in the genital area. Careful history taking, examination, and confirmatory testing enabled the prompt diagnosis of syphilis and mpox co‐infection. The input from the social worker and the public health unit facilitated the vaccination of close contacts and the prevention of further infections.
Lessons from practice
- Mpox, syphilis and genital herpes should be considered in at‐risk patients presenting with genital ulcers, as co‐infection may be present.
- A detailed sexual and travel history is important to narrow down the differential diagnosis.
- Careful examination and appropriate sampling for testing and consideration of presumptive treatment for syphilis and herpes simplex virus are crucial before isolation of the patient if mpox is suspected.
- Information provision in the patients' language and liaison with the public health unit is essential in contact tracing and provision of patient‐centred care for mpox.
Box – Cluster of coalescing ulcers with black scabbing and surrounding erythema in pubic area (A); single painless ulcer with induration and a healing base on the underside of the penis at the penoscrotal junction (B)
Comments
Post a Comment