H1N1 Influenza (Swine Flu): Practice Essentials, Background, Epidemiology - Medscape Reference
Swine influenza is a highly contagious respiratory disease in pigs caused by one of several swine influenza A viruses, as recently reviewed. [1, 2] In addition, influenza C viruses may also cause illness in swine. Strategies to control swine influenza virus (SIV) in animals typically include one of several commercially available bivalent swine influenza virus vaccines.
Transmission of swine influenza viruses to humans is uncommon. However, the swine influenza virus can be transmitted to humans via contact with infected pigs or environments contaminated with swine influenza viruses. Once a human becomes infected, he or she then can spread the virus to other humans, presumably in the same way as seasonal influenza is spread (ie, via coughing or sneezing).
History
The ability to trace outbreaks of swine flu in humans dates back to investigation of the 1918 Spanish influenza pandemic, which infected one third of the world's population (an estimated 500 million people) and caused approximately 50 million deaths. In 1918, the cause of human influenza and its links to avian and swine influenza was not understood. The answers did not begin to emerge until the 1930s, when related influenza viruses (now known as H1N1 viruses) were isolated from pigs and then humans. [6]
In humans, the severity of swine influenza can vary from mild to severe. From 2005 until January 2009, 12 human cases of swine flu were reported in the United States; none were fatal. In 1988, however, a previously healthy 32-year-old pregnant woman in Wisconsin died of pneumonia as a complication of swine influenza.
A 1976 outbreak of swine influenza in Fort Dix, New Jersey, involved more than 200 cases, some of them severe, and one death. [7] The first discovered case involved a soldier at Fort Dix who complained of feeling weak and tired. He died the next day.
The fear of an influenza pandemic in 1976 led to a national campaign in the United States designed to immunize nearly the entire population. In October 1976, approximately 40 million people received the A/NewJersey/1976/H1N1 vaccine (ie, swine flu vaccine) before the immunization initiative was halted because of the strong association between the vaccine and Guillain-Barré syndrome (GBS). [8, 9] About 500 cases of GBS were reported, with 25 deaths due to associated pulmonary complications. [10]
A recent investigation sought to determine the link between GBS and the 1976 swine flu vaccine, because subsequent influenza vaccines did not have this strong association. Nachamkin et al found that inoculation of the 1976 swine flu vaccine, as well as the 1991-1992 and 2004-2005 influenza vaccines, into mice prompted production of antibodies to antiganglioside (anti-GM1), which are associated with the development of GBS. They proposed that further research regarding influenza vaccine components is warranted to determine how these components elicit antiganglioside effects. [11]
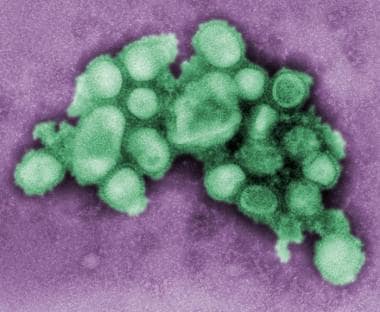 This preliminary negative stained transmission electron micrograph depicts some of the ultrastructural morphology of the A/CA/4/09 swine flu virus. Courtesy of CDC/ C. S. Goldsmith and A. Balish.
This preliminary negative stained transmission electron micrograph depicts some of the ultrastructural morphology of the A/CA/4/09 swine flu virus. Courtesy of CDC/ C. S. Goldsmith and A. Balish. 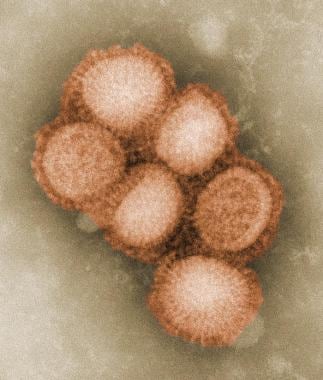 This preliminary negative stained transmission electron micrograph depicts some of the ultrastructural morphology of the A/CA/4/09 swine flu virus. Courtesy of CDC/ C. S. Goldsmith and A. Balish.
This preliminary negative stained transmission electron micrograph depicts some of the ultrastructural morphology of the A/CA/4/09 swine flu virus. Courtesy of CDC/ C. S. Goldsmith and A. Balish. 2009-2010 H1N1 influenza (formerly called swine influenza) outbreak
Human cases of influenza A (H1N1) were reported worldwide. In 2009, cases of influenzalike illness were first reported in Mexico on March 18; the outbreak was subsequently confirmed as H1N1 influenza A. [12] Suspected clinical cases had been reported in 19 of the country's 32 states, although only 97 of the Mexican cases had been laboratory-confirmed as influenza A/H1N1 [13] (12 of them genetically identical to influenza A/H1N1 viruses from California. [12] ) As of May 5th, 2009, nearly 600 H1N1 influenza cases had been confirmed in Mexico, including 25 deaths. [14]
On April 17, 2009, the CDC determined that 2 cases of febrile respiratory illness in children who resided in adjacent counties in southern California were caused by infection with a swine influenza A (H1N1) virus. [15] By April 26, 2009, the US Department of Health and Human Services (HHS) declared a national public health emergency involving H1N1 influenza A, citing its significant potential to affect national security. [16] By June 25, 2009, 27,717 lab-defined cases of H1N1 influenza had been confirmed in the United States. [13, 17, 18, 19]
Estimates in the United States for the first 6 months of the pandemic reported approximately 22 million people in the United States became ill from the H1N1 influenza, nearly 100,000 were hospitalized, and about 3900 died. Deaths include an estimated 540 children younger than 18 years, 2900 adults aged 18-64 years, and about 440 elderly individuals. These estimates are from the CDC's Emerging Infection Program, rather than using only laboratory-confirmed cases. [20]
For an updated tally and case counts in specific states, see the CDC's H1N1 Flu (Swine Flu) Web page.
On June 11, 2009, the WHO raised the pandemic alert level to phase 6 (indicating a global pandemic) because of widespread infection beyond North America to Australia, the United Kingdom, Argentina, Chile, Spain, and Japan. [13] As of September 1, 2009, the WHO reported that H1N1 influenza had been confirmed in over 200,000 people in more than 100 countries and that they were aware of at least 2185 confirmed deaths. For an updated tally of affected countries and counts, see WHO's Influenza A (H1N1) Web page.
On October 24, 2009, President Obama declared the 2009 H1N1 influenza pandemic a national emergency, explaining that "...the rapid increase in illness across the Nation may overburden health care resources and that the temporary waiver of certain standard Federal requirements may be warranted in order to enable U.S. health care facilities to implement emergency operations plans, the in the United States 2009 H1N1 influenza pandemic constitutes a national emergency." This declaration made way for waiving certain requirements of the Medicare, Medicaid, and State Children's Health Insurance programs and of the Health Insurance Portability and Accountability Act Privacy Rule throughout the duration of the public health emergency. [21]
Government and public health officials are monitoring this situation worldwide to assess the threat from H1N1 influenza and to provide guidance to health care professionals and the public. Because the situation is changing rapidly, it is important to check regularly for changes in recommendations as new information becomes available. Online resources for daily guidance include the Centers for Disease Control and Prevention (CDC), World Health Organization (WHO), and Medscape's H1N1 Influenza A (Swine Flu) Alert Center.
Domínguez-Cherit et al (2009) conducted an observational study of consecutive critically ill patients in Mexican hospitals that treated most patients with confirmed, probable, or suspected H1N1 influenza during the 2009 epidemic. Critical illness occurred in 58 (6.5%) of 899 patients. The median age of critically ill patients was 44 years (range, 10-83 y). All presented with fever, and all but one with respiratory symptoms. Few patients had comorbid respiratory disorders, but 36% were obese. All patients but 2 received mechanical ventilation for severe acute respiratory distress syndrome and refractory hypoxemia. By 60 days, 24 patients had died (41.4%). Patients who died had greater initial severity of illness, worse hypoxemia, higher creatine kinase and creatinine levels, and ongoing organ dysfunction. Treatment with neuraminidase inhibitors was associated with improved survival (odds ratio, 8.5). [22]
See Medscape's H1N1 influenza algorithm adaptation for guidance in managing suspected cases.
A WHO report on the 2009 influenza pandemic indicated that nearly all countries reported cases of H1N1 virus infection, with more than 17,000 deaths worldwide. In the United States, the number of clinical illnesses was estimated at 59 million, 265,000 hospitalizations, and 12,000 deaths. [23] H1N1 strains are still prevalent in India, whose Health Ministry has reported over 2500 deaths to date.
In the second half of 2011, a novel swine influenza virus emerged. Twelve cases from 5 states were reported by the CDC in January 2012. The new strain, dubbed A (H3N2)v, includes a gene from the human pandemic strain and affects mostly children. In 3 of the 5 states where the virus emerged (Pennsylvania, Maine, and Indiana), the virus was a result of pig-to-human transmission. [24]
Comments
Post a Comment